Hi friends!
Today is the second anniversary of my first (of 3) lipedema removal surgeries with Dr. Jaime Schwartz in California. (I detail all of my surgery recoveries day by day on my YouTube channel if you’d like to hear me discuss more.)
So, I still need more surgeries – the next one is a big one that will require significant recovery time because it’s the abdomen. The purpose of this is to remove diseased tissue from pushing on my lymph nodes in the groin and hopefully, release lymphedema from my left leg. So far, I’m not mentally prepared to continue surgeries.
In the last two years, I’ve been very dedicated to swimming as much as I can, wearing compression, and daily Manual Lymphatic Drainage. I’ve used a prescription-grade FlexiTouch Pneumatic Pump as a last-resort, backup plan on flare days, and on days when I cannot get to the swimming pool. I continue to perform sedentary work but have retired from a very stressful management job that required extensive travel within the last month.
Observations
A lot of nodules that I could both see and feel in the groin, and on the fat pads on the inside of each knee were removed. These nodules hurt me daily, affected my gait, and I believe, would have continued to grow. When I palpate the knees, I do not feel nodules now. When I palpate the upper thigh, I feel a new nodule the size of a pinto bean that’s been there for a few months.
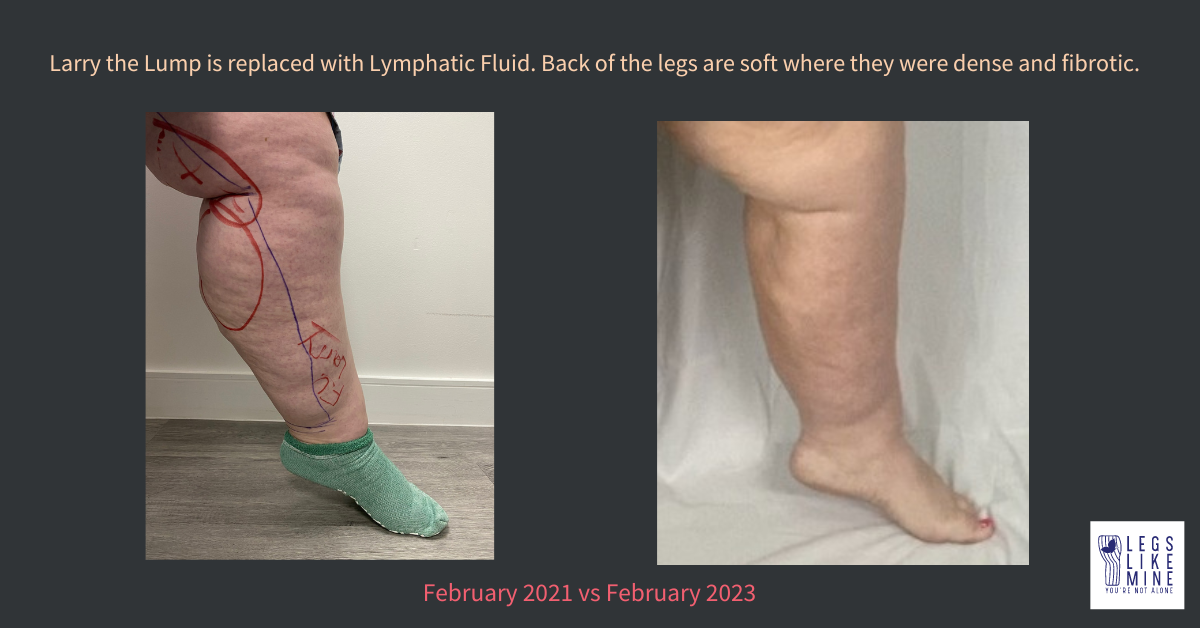
I had extremely dense and painful fibrosis on the back and inner part of both calves before surgery. That was removed during my first surgery and the pain in the back of my legs is totally gone. It hurt me all night, every night pre-surgery. Also, my calves touched and rubbed when I walked, where now they do not make contact when walking. This is a tremendous improvement in my mobility.

On the inside of my left leg was a tremendous nodule I’d named Larry, pre-surgery. It was removed without a skin removal. That area has filled with lymphatic fluid that I massage several times a day and wrap (on top of compression) most days. I believe it is at risk of turning into a cuff or fold if swelling gets out of control, so that inspires me to wear compression there as often as is possible. I need more surgery in this area, but it is far down the priority list.
[Note: there is a paper out now by Dr. Karen Herbst, reporting that some women are experiencing lymphedema after liposuction for lipedema treatment. I’ll cite that below for you to read up on.]
The fronts of my thighs have remained empty, and there is some loose skin. However, when I wear compression under clothing, this area is so much better looking cosmetically. Also, my ability to walk is greatly improved due to removal of the diseased tissue in this area.

The Unintended Consequences
The downside (and it’s a big one) is that my knee nodules and fat pads had grown large over the years, and pushed out, even stretching the connective tissues in my knees. Once the pads were less dense, the connective tissues were still stretched. While I know I have hypermobility (a very common co-disease with lipedema), it was enhanced tenfold once the fat pads were not a factor. My knees dislocate painfully sometimes as much as several times a day. Recently they’ve started “locking” in place, immobilizing me until I can figure out how to ease them into a moveable position. I’ve been getting steroid injections in my knees, but my orthopedic doctor has advised I will need two complete knee replacements sooner than later, due to the damage that my knees have taken on since fat pad removal. I’m trying to delay this surgery as much as possible. Right now, I am 49 and relatively active, so I don’t want to repeat a knee replacement when I’m 75 if I can avoid it.
What Action I’m Taking
In addition to swimming, I see a physical therapist regularly and we are working to strengthen core, hip, calf, etc. muscles in order to prepare my body to be in the best shape possible for knee replacement. I faithfully do the exercises at home and have rejoined a gym to do some of the exercises requiring weight machines without the added benefit of an insurance copay ($30 per PT visit in my case). I continue to struggle with sugar consumption and try each day to do more to clean up my diet in a consistent way.
I use a cream called Voltaren on my knees for effective pain relief, and I also take Tylenol for knee pain regularly. Additionally, my PT ordered me a TENS unit for at home use on anything that hurts, and I’ve been using it on my right knee, which has been totally locking up lately, each night for 40 minutes. According to tensunits.com, “TENS (Transcutaneous Electrical Nerve Stimulation) is a small machine with electrodes that send stimulating pulses along nerve strands and across the skin’s surface. These impulses help to reduce pain by encouraging the body to produce more endorphins, which act as a natural painkiller.”
I’ve started very gentle, lowest-setting, use of a vibration plate in a seated position only due to my knee issues, 4 times a week in 15-minute sessions, to continue to move lymphatic fluid. Finally, I mentioned I use compression wraps as needed. I also see an occupational therapist, who will be bandaging my lymphedema to get it back under control in my next visit.
I think that’s it for now. A lot to think about if you’re considering surgery as a stage 3 or 4 lipedema patient. The surgery is not going to stop the disease, but it will get rid of painful, diseased tissue and nodules. It certainly isn’t a cosmetic surgery, because in some ways, I actually look worse than before. But the pain is SO much better, and my gait is so much better. It’s been good overall, but there are side effects to know about. I suspect some of them were coming one way or another (knee replacement), but maybe later, had I not had the lipedema removed.
I hope this helps someone in their journey. Until next time, stay well!
Susan
Sources:
The Ehlers-Danlos Society. Assessing Joint Hypermobility – The Ehlers Danlos Society (ehlers-danlos.com).
The Original Tens Units.com. How does a Tens Unit work? www.TensUnits.com/pages/how-does-a-tens-unit-work.
Wright TF, Herbst KL. A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema. Am J Case Rep. 2022 Jul 11;23:e935016. doi: 10.12659/AJCR.935016. PMID: 35811389; PMCID: PMC9284075.
Includes paid ads. As an Amazon Associate, I receive compensation for sales.