Hi friends!
I’m continuing my series of downloading good things from the Lipedema World Congress that was in Potsdam Germany a couple of weeks ago. Here is a link to the program for reference: LWC_Program_web.pdf (lipedema-world-congress.com). Also note, the second world congress will be in two years in Rome, and patients are welcome. So get ready for that. I do love Rome.
It’s got to be totally by design that the presentation that was my favorite was also the very first at the Congress, and it was even given before the opening and welcome speeches – it’s important.
Given by a lovely nurse named Christine Moffat from the International Lymphoedema Framework. This presentation had several key points that all lead up to one thing: it’s all about how you treat and listen to patients, so stop making them feel guilty because they have lipedema.
I actually sat and typed up my notes in kind of a raw format, and I’m sharing with you my raw notes (almost word for word as she talked) so you can read them yourselves. I love how she sat the tone for the whole Congress with this lovingly-delivered speech:
Raw Transcript Notes
- She is a nurse. Wants to move the field forward in a good way.
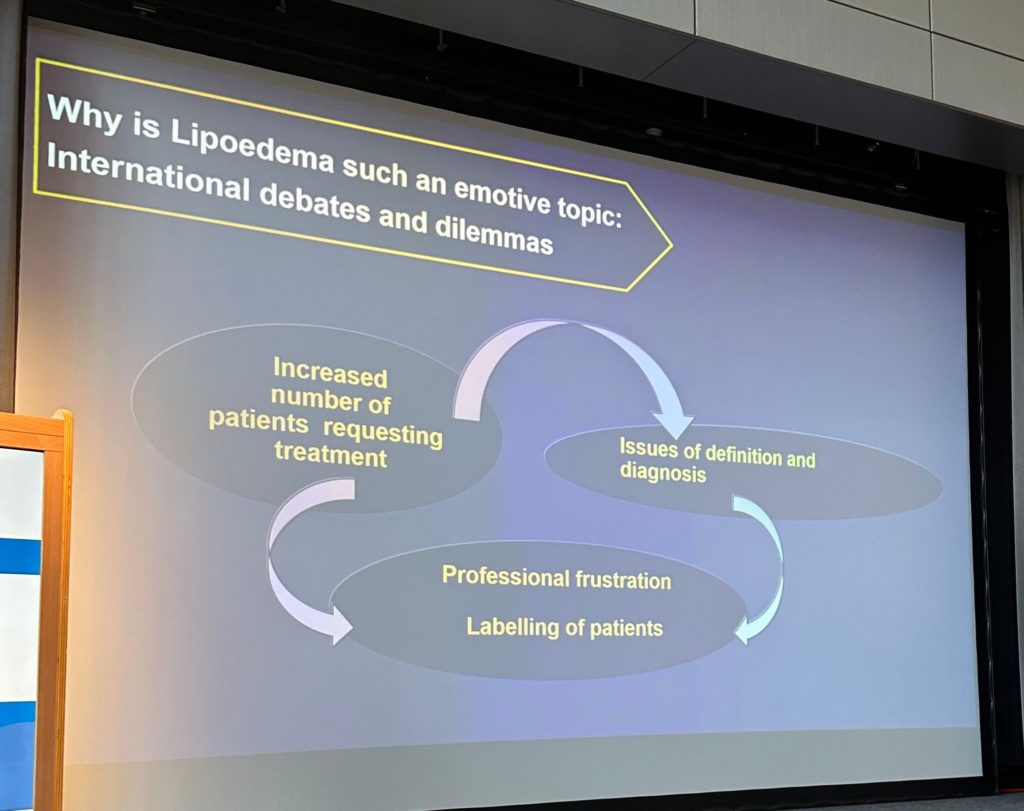
- Why is lipedema an emotive topic – international debates and dilemmas? There’s an elephant in the room.
- Increased number of patients requesting treatment
- Issues of definition and diagnosis
- Professional frustration with labeling of patients
- Come in with obesity, breast cancer, and other presentations and other conditions
- Facing the reality of trying to get treatment.
- Why are we here today? There is a world recognition that we must come to grips on this topic.
- Other scientists doing this group and we need to come together
- We need to define what we’re talking about, what it is, and what it isn’t
- We don’t have a set of diagnostics to help us with this. No diagnostic test that we can use, leads to clinicians saying it’s all in our head, go away
- Combined international frustration. Don’t know how or where to help.
- Big danger or labeling patients in an unhelpful way.
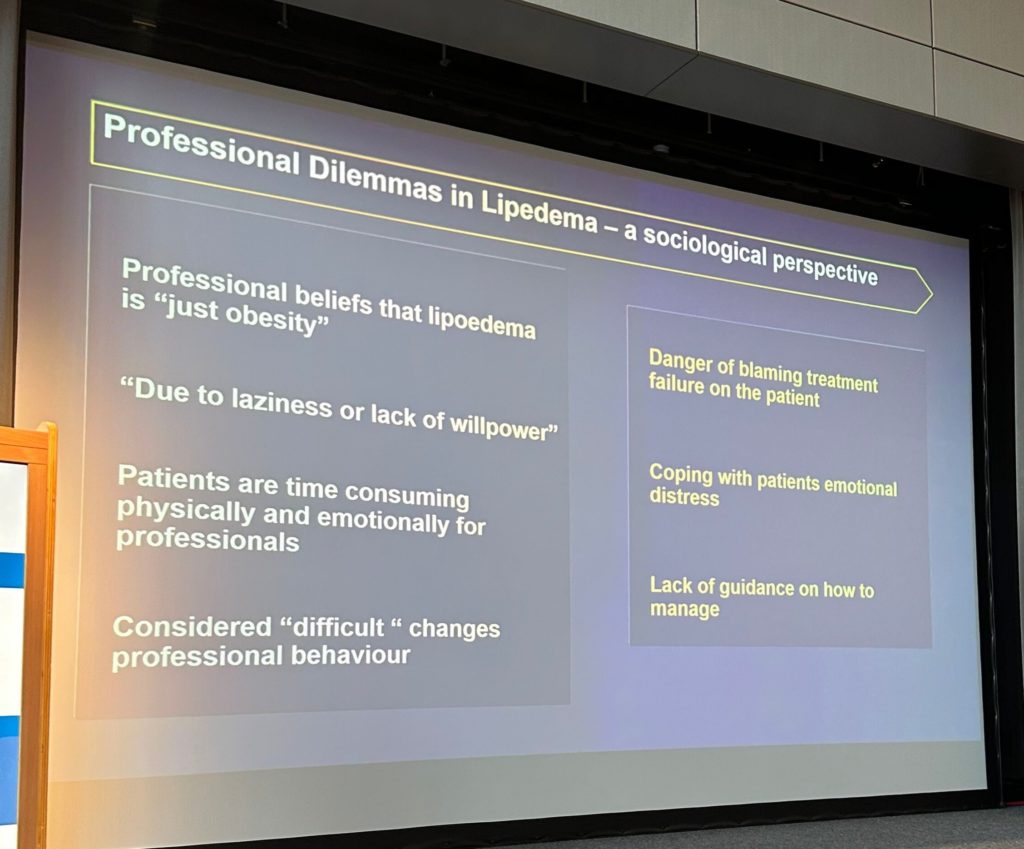
- Description of things – one of the most unhelpful things we do is label inappropriately. Lipedema is just obesity. Labeling someone brings a lot of blame on them.
- Clinicians that say you’re just lazy and lack willpower. That’s not right when we are in the midst of daily life.
- Patients are time-consuming physically and emotionally and professionally. Emotional labor for clinicians.
- We are often considered difficult patients – the heart sink patients.
- When we label, we predetermine treatment and relationships, letters like noncompliance in medical notes will affect how professionals look at patients when they see the notes in medical files.
- Patients can decide on the therapeutic relationship within first minute. Will they feel empathy and compassion? We must be active listeners. Professional response can determine how patients feels.
- Want to get patients away from thinking they should be shamed about their condition as shame turns into guilt. This is the heart of the successful therapeutic relationships.
- Pain can be the most distressing part of lipedema. Pain management should be a priority. Need to understand that there is pain even though there may not be test evidence.
- When we listen people start to heal the moment they feel heard.
- Pain assessment must be done – not an option. Needs to be rigorous or standardized, think about the spectrum of issues and identify the intensity and belief systems about their condition. This also affects the emotional side.
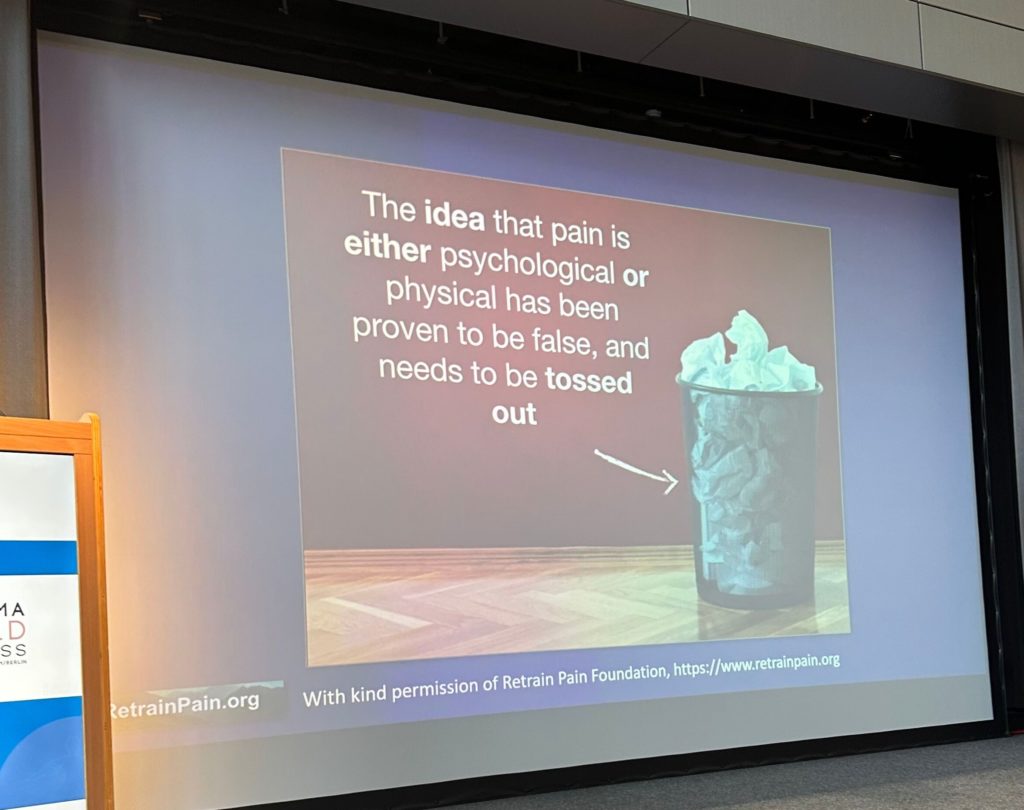
- Smash the idea that pain is either psychological or physical has proven to be false and needs to be tossed out.
- Realize that our treatments can change the pain.
- What do we need to think about?
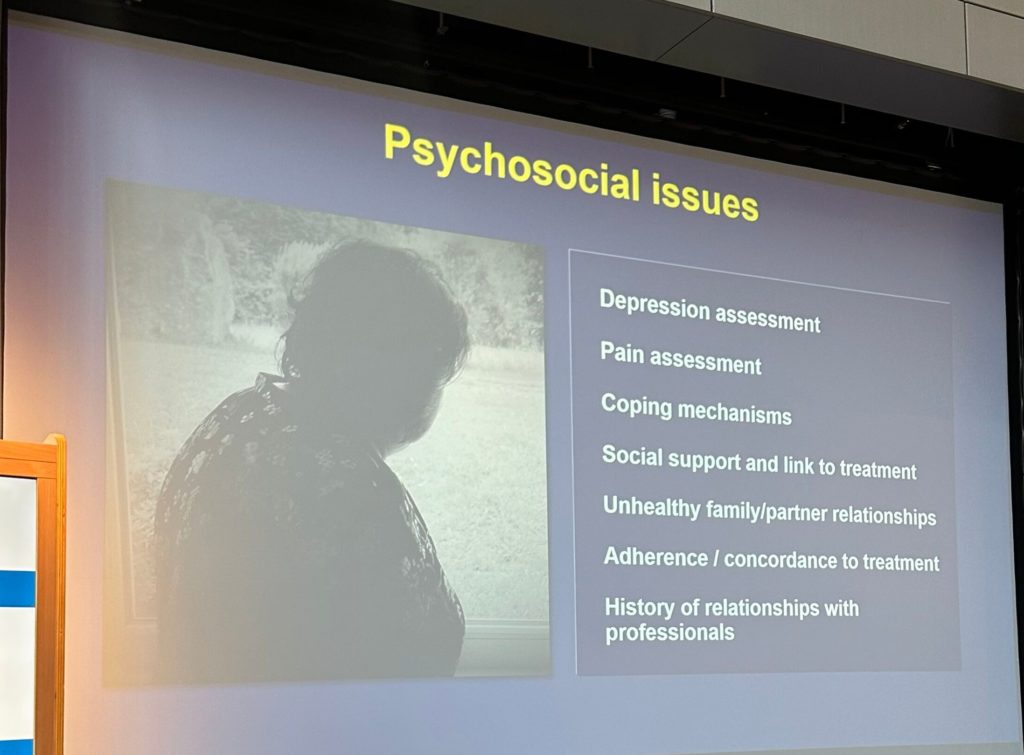
- Depression, coping, pain assessment, coping mechanisms, social support and link to treatment, unhealthy family partner relationships, adherence, concordance to treatment, history of relationships with professionals.
- Don’t always think about what the doctor the patient can comply due to all of the other things in the patient situation. A lot of this is obscured by the history of patient relationships with clinicians.
- Reinforces that the psychosocial area has so much to do with compliance. Need to understand the full picture and set achievable goals for that particular patient.
- Don’t want patients to have unrealistic attitudes about the cure.
- We do want to embrace self-management to have healthier lives.
- Physicians and therapists play a key role in supporting self-management. Listen to each other, debate, and have different ideas but there is a necessity to listen and move together.
- She is with the ILF. Don’t claim to know all the answers and try to keep a sense of openness to learn together and appreciate that in ten years the science will be moved on.
- Stop telling patients they need to stop being guilty about lipedema and obesity. Support them through therapeutic relationships of trust, and provide compassionate supportive care, understand treatment options and when it’s right to invoke the wider team.
- We are opening a door for them. They need hope and a lot of strength to carry on. Every patient that comes to us can have something we can do, even holding a hand to surgery. We can and must focus on hope and strength.
- We are stronger together.
I love this.
Susan