Hi friends!
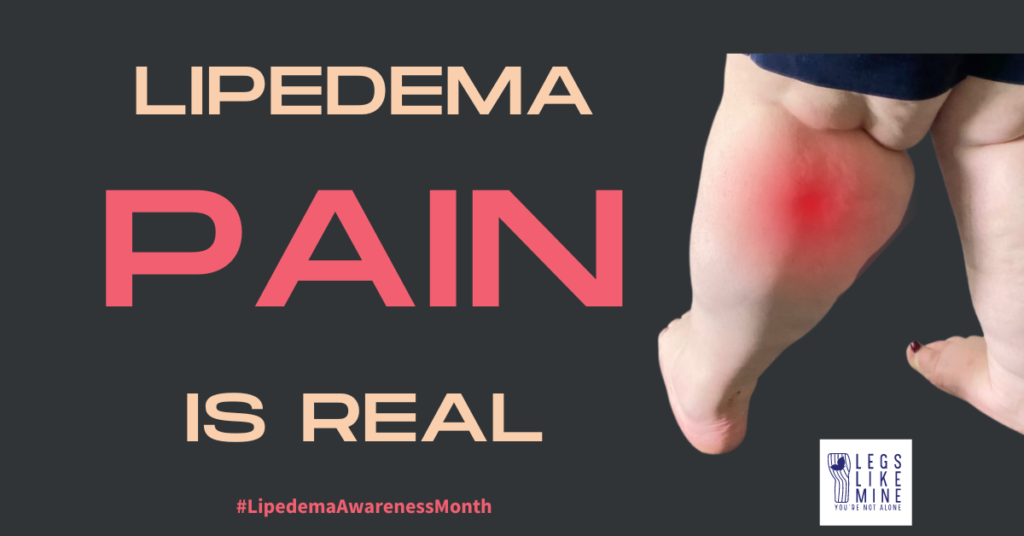
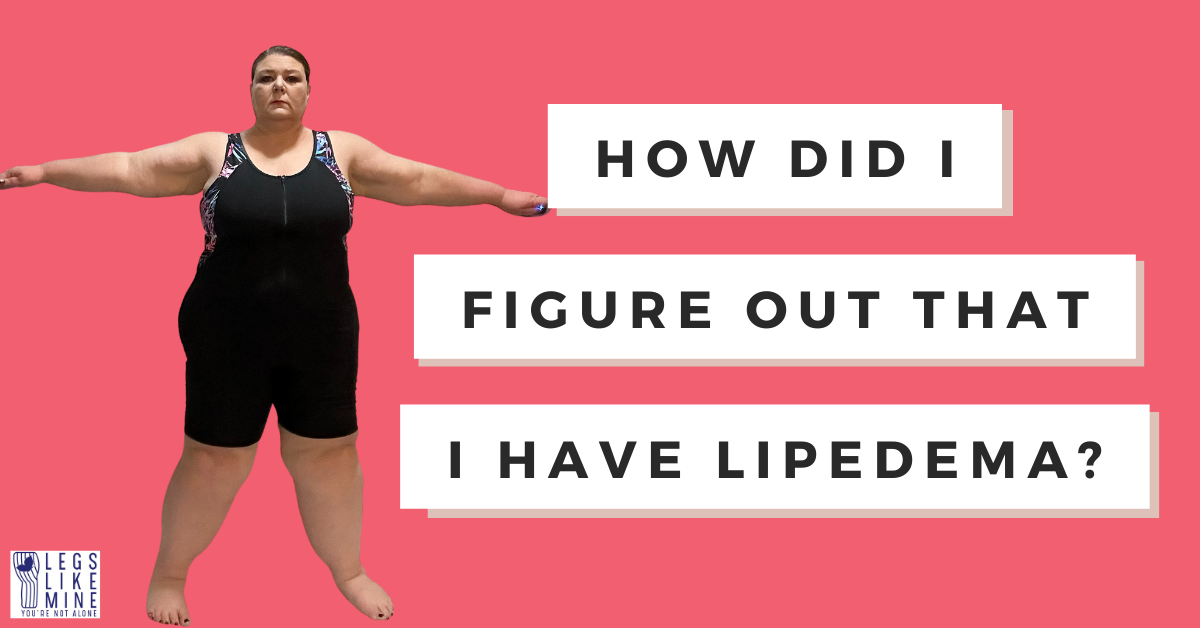
Today, I want to address a topic that is often overlooked or misunderstood, can’t be seen and maybe…(?) isn’t always believed. PAIN – the physical pain experienced by those living with lipedema. This chronic condition, characterized by the disproportionate accumulation of fat in the legs and sometimes arms, is WAY more than just a cosmetic concern. It is a source of constant discomfort, aching, and at times, excruciating pain.

I use a vibration plate to help alleviate pain. It actually feels really good. I use mine while seated because my knees need replacing.
As someone who is not only a lipedema patient but has also witnessed the struggles of hundreds of lipedema patients firsthand, I cannot emphasize enough the importance of validating and acknowledging lipedema pain. It is real, it is debilitating, and it deserves our utmost attention and empathy.
Research Validates the Pain
Numerous studies have shed light on the prevalence and severity of pain experienced by individuals with lipedema. One such study, published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders, found that a staggering 87% of lipedema patients reported experiencing pain, with over half rating their pain as severe.
Another study, published in the Journal of Lymphoedema, highlighted the significant impact of lipedema-related pain on quality of life. The researchers found that pain was a major contributor to reduced mobility, impaired daily activities, and increased psychological distress.
These findings are further supported by a systematic review published in the Journal of Obesity, which analyzed multiple studies on lipedema and its associated symptoms. The review concluded that pain is a common and often debilitating symptom, with many patients reporting chronic, widespread pain that worsens with disease progression.
How Does My Personal Pain Feel?
For me, I live a pretty active lifestyle, and I’m not planning to slow down but I’ve definitely had to make modifications. But I also have to temper that these days. My pain sources are in two places, one is my calves (which I’ve already had several surgeries on, but am not done). It usually hits in the night during bedtime, and then for a full day after big walking or lots of standing. It definitely wakes me up and can range from a dull aching to an all over the calf scream for help. The second part of my pain is related to my joint hypermobility, which increased significantly after I had surgery to remove a lot of the fat pads around my inner knees. If I take stairs, even just a few, I will pay…dearly the next day. If I’m lucky enough to not have a dislocation or subluxation during stair taking, I’ll have a full day of recovery involving ice, voltaren (cream for pain), and pain meds to knock of the I’d say level 8-9 pain on a 10 point scale. Now if I have a subluxation (happens frequently when going down stairs), I’ll be at a ten for a couple of days in the joint area. Add that on top of the calf pain (which is definitely less after having a lot of fibrotic tissue removed from my legs so far, but still I’d say a 5-6/10 on bad nights).
Emotionally, I hate it. I’m independent to a fault, and I hate being limited by having to avoid certain activities or finding the elevator all the time. But even though I CAN do the stairs, I SHOULD NOT do the stairs, if that makes sense. Because I will pay for it big time. And every time I go down stairs, I risk a subluxation and a fall, so that would be bad.
A Call for Understanding and Empathy
To those living with lipedema, I want you to know that your pain is valid, and you are not alone. Your struggles are real, and they deserve to be acknowledged and addressed.
To friends, family members, caregivers, and medical professionals, I urge you to listen with open hearts and minds. Lipedema is not just a cosmetic issue; it is a condition that causes significant physical and emotional distress. Dismissing or minimizing the pain experienced by these individuals is not only insensitive but also perpetuates the stigma and misunderstanding surrounding this condition.
Let us come together as a community, united in our efforts to raise awareness, promote understanding, and advocate for better support and treatment options for those living with lipedema.
One Other Point – People Who’ve Had Liposuction/Lipedema Removal May Still Have Pain. Don’t Make Assumptions
My personal experience is that my calf pain went down but is still there (I will always have lipedema) after some of the fibrosis was removed. But my joint pain greatly increased with the removal of fat pads, that I’m thinking were stabilizing my knees. So when you see people whose legs appear to be “normal” (whatever that is), remember they may still be suffering from issues leftover and created by lipedema and its comorbidities like hypermobility.
Tips for Avoiding and Managing Lipedema and Hypermobility Pain
- Wear compression garments like stockings or leggings to reduce swelling and improve circulation. For me, if I know I’m going to be standing all day or travelling, I wear my best compression, and even double up. (Talk to your doctor to make sure you’re OK for compression.)
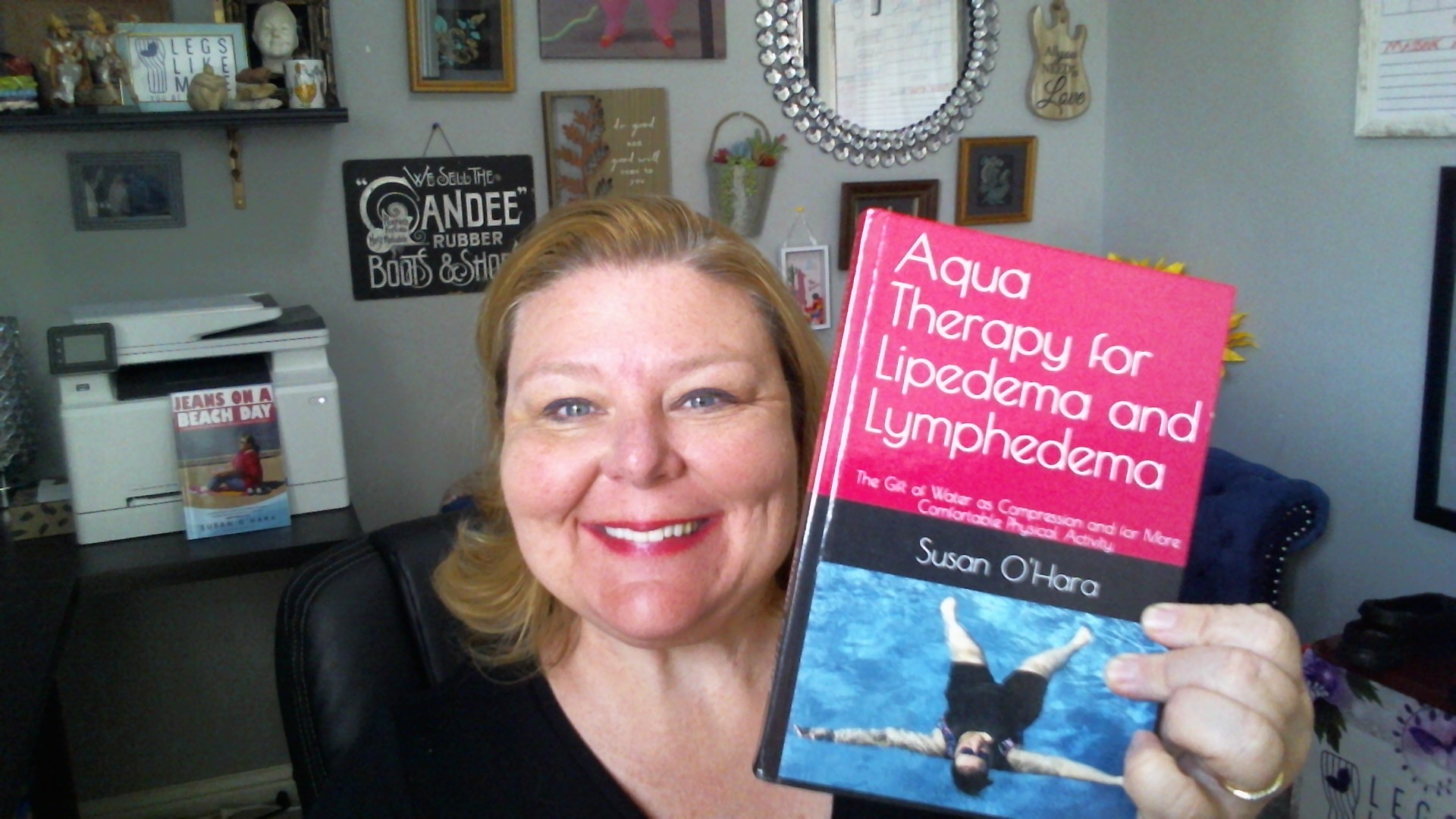
- Engage in regular exercise like swimming to strengthen muscles and improve circulation
- Follow an anti-inflammatory diet to reduce inflammation. That may mean finding out what foods trigger swelling for you and avoiding them, or doing with a generic list of anti-inflammatory foods to add some to your diet
- Elevate your legs as often as you can to avoid swelling, because swelling can cause pain
- Use manual lymphatic drainage massage to stimulate lymph flow around blocked areas
- Switch positions frequently. Avoid standing or sitting for long periods to prevent fluid buildup
- Apply moisturizers to prevent dry skin. I do this in the evenings after compression is off for the day so I don’t damage compression fibers
- Avoid very hot water over 94 degrees, as direct exposure to this level of heat can make symptoms and pain worse in many
- Consider using ice packs for 15 minutes off and on in areas that are really problematic
- Talk with your doctor about pain meds and external pain creams and how they might complement your situation

This is the kind of cream I use on my joints and calves when they’re really bad. Talk with your doctor first.
Call to Action
If you or someone you know is struggling with lipedema-related pain, I encourage you to seek support and guidance from healthcare professionals who specialize in this condition. Additionally, consider joining support groups or connecting with others who understand your journey – their shared experiences and empathy can be invaluable.
To those who have the privilege of being allies, I implore you to educate yourselves, listen without judgment, and offer compassion and understanding. Small acts of kindness and empathy can make a world of difference in the lives of those battling this often-misunderstood condition.
Together, we can create a more inclusive and supportive environment for lipedema patients, acknowledging their pain, and working towards better treatment options and improved quality of life.
Remember, pain is not just a physical experience; it can affect every aspect of someone’s life. Let’s commit to validating and alleviating the suffering of those living with lipedema.
Stay well friends, and don’t be afraid to take the elevator to save yourself a day of pain.
Susan
For More Information
Check out the Lipedema Foundation’s article on pain. https://www.lipedema.org/blog/2023/4/12/lipedema-pain-what-do-we-know
Sources:
Buso, G., Depairon, M., Tomson, D., Raffoul, W., Vettor, R., & Manzato, E. (2019). Lipedema: A Call to Action! Similarity with Pitting Edema in Stem Endings. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 7(5), 656-664. https://doi.org/10.1016/j.jvsv.2019.03.001
Fetzer, A., & Wise, C. (2015). Living with Lipoedema: Reviewing Treatment Strategy and Addressing Unmet Needs. Journal of Lymphoedema, 10(2), 10-19. https://www.theprimeinstitute.org/wp-content/uploads/2016/06/Fetzer-Wise-2015.pdf
Fife, C. E., Maus, E. A., & Carter, M. J. (2010). Lipedema: A Frequently Misdiagnosed and Misunderstood Fatty Deposition Syndrome. Advances in Skin & Wound Care, 23(2), 81-92. https://doi.org/10.1097/01.ASW.0000363503.92694.93
Contains paid ads. As an Amazon Associate I receive earnings for your purchases.